Click the link to learn more and register:
https://docs.google.com/forms/d/e/1FAIpQLSeeQ1dm2KjwhU9717hHz287NuHvxF8oamuIJrchLiGnt0CCpw/viewform

Click the link to learn more and register:
https://docs.google.com/forms/d/e/1FAIpQLSeeQ1dm2KjwhU9717hHz287NuHvxF8oamuIJrchLiGnt0CCpw/viewform

link to supporting article: https://rdcu.be/c277G

Registration is up: https://cmelearning.usask.ca/final_sono22_marketing-poster_accred-approved.pdf
We’re offering 3 hours of supervised scanning in the afternoon – spots limited to 24 participants.
Check it out – new team delivering POCUS courses in Saskatchewan. More dates for Regina & Saskatoon coming soon!

PoCUS Courses

This year we’re hosting a POCUS educator’s summit – a SONO-SUMMIT!
With increasing demands for POCUS training within the medical education spectrum, there are growing calls for guidance on curricular aspects like choosing what to teach, how to assess it, and how to define and determine competence in POCUS at all stages of training. Overall learner objectives include presenting the best available medical education evidence on POCUS in UGME, PGME and CME.
Lectures
1) Best practices/evidence in UGME POCUS highlighting the Canadian Medical Students’ Ultrasound Curriculum (CanUCME group) as well as exploring key challenges including integration into the broader curriculum, equipment needs, and assessment. Link to the article found here!
2) Best practices/evidence in PGME POCUS with focus on competency based medical education (CBME) including entrustable professional activities, assessment with entrustment scores, and competency committees. Link to the Ultrasound Competency Assessment Tool validation found here!
3) Best practices/evidence in CME POCUS highlighting the need for longitudinal learning opportunities with CME recognition, supervision (both direct and indirect), scanning bootcamps, and the role of assessment for credentialing.
Our Faculty

From Top Left Clockwise: Dr. Michelle Clunie, Dr. Paul Olszynski, Dr. Dan Kim, Dr. Gillian Sheppard, Dr. Irene Ma, Dr. Colin Bell
Workshops
Each of the three main topics will be followed by a set of interactive workshops/break-out rooms (virtual) helping participants put ideas to paper/laptop while also getting a chance to ask/discuss challenges or questions with our experts. Workshops will include topics such as: Giving a good POCUS lecture, Teaching POCUS during clinical work, Preparing POCUS curriculum proposals, Using POCUS assessment tools, Completing EPA scores and narratives.
Save the date: Saturday morning, April 17th, 2021. Registration coming soon!

Clinical Ultrasonography (aka Point of Care Ultrasound or POCUS) is broad in scope and its clinical applications are far-reaching. As early as 2014, half of Canadian medical schools had already implemented some form of clinical ultrasound education into their undergraduate medical education (UGME) programing (1). Six years later, national standards have yet to be established. Educators at the undergraduate medical level are struggling to determine what ultrasound skills to include, exclude, or defer to residency – a challenging balance given an already crowded UGME curriculum. Clearly, there is a need for national curricular guidelines in clinical ultrasonography. Accordingly, the Canadian Ultrasound Consensus for Undergraduate Medical Education (CanUCMe) group was formed in 2018 comprising 21 ultrasound experts and educational leaders from 15/17 Canadian medical schools (2). CanUCMe’s experts aimed to determine which curricular objectives should be taught to ensure a foundational understanding of clinical ultrasonography. Using a modified Delphi method, these experts submitted their recommendations for curricular goals and after three rounds of rigorous review and voting, the group reached consensus on 85 ultrasound objectives to include as minimum requirements at the UGME level.
The University of Saskatchewan’s UGME ultrasound curriculum is now in its 6th year. As such, it seems appropriate to check in and evaluate our program alongside CanUCME’s proposed standards and objectives. This review was undertaken by the authors, medical students at USask. It includes a comprehensive review of all clinical ultrasound education throughout pre-clerskship and clerkship, as well as a review of all program evaluations over the past 5 years. This article was peer reviewed by both USASK Faculty as well as external experts for accuracy and clarity.
Ultrasound-Guided Medical Education (the other UGME!)
The USASK UGME ultrasound curriculum includes educational US in the Anatomy course in first term, followed by induction into clinical US in the clinical skills courses of terms 2 through 4. This exposure in pre-clerkship translates to ~ 9 hours of hands-on supervised US training. Clerkship exposure is rooted in the core EM rotation, but is also found on other services to varying degrees .While introducing a skill such as ultrasound can be challenging, the transition from didactic lectures to learning practical skills is well facilitated through a flipped-classroom model that includes video tutorials and hands-on scanning sessions with standardized patients and an interprofessional team of instructors (physicians, nurses, paramedics). Student group sizes during scanning sessions are kept small (typically 2-4 students to each machine/patient) in an effort to maximize hands-on scanning time for each learner.

The curriculum is designed to enhance longitudinal learning of the curricular elements through spaced repetition and practice. 37 elements are revisited in pre-clerkship and only 7 elements are not re-visited in clerkship. With 92% of students passing their POCUS OSCE (able to perform the scan with little to no prompting, OSCE results for MS2 class, 2017), the U of S ultrasound curriculum appears to be effective at achieving foundational POCUS skills.
Things USASK does well
As indicated in evaluative feedback forms, students are happy with the bedside preceptors as their supportive attitude enables students to comfortably experiment with ultrasound. We believe that this is crucial when learning a spatially challenging practical skill. Additionally, preceptors have extensive POCUS experience and can challenge students to think about what they are doing from a clinical perspective. Finally, students find that groups are small enough that they are still able to receive individually tailored feedback while also learning from watching their peers and discussing skills as a group.

The USASK ultrasound curriculum meets 77 (90%) of the final 85 Consensus-Based Recommended Curricular Elements for Ultrasound in Canadian UGME. Indeed, only 12 of the 85 elements are not met during pre-clerkship years 1 and 2, with four of those being later introduced in clerkship, leaving 8 elements: ALARA, potential bioeffects, proximal inguinal regional vessels, heart sound generation in physiology, consolidation, ultrasound-guided peripheral intravenous insertion, general needle guidance technique using ultrasound, and use of small-group scanning on patients. The U of S ultrasound curriculum appears to be effective at achieving the desired curricular elements. in addition to providing a welcoming environment for medical students to learn ultrasound.

Clerkship students are also eligible to apply for the Clinical Ultrasound Elective in Clerkship (CUSEC) in their second year of clerkship. This is a 2-week intensive rotation which includes a competency assessment. The first week is non-clinical and focuses on hands-on scanning time as well as seminars which have received exceptional feedback. The second week allows the students to choose a rotation/discipline and develop an approach to integrating ultrasonography into everyday care (3). All but one element – “heart sound generation” – are subsequently covered in the 4th year Clinical UltraSound Elective in Clerkship.
More Than Meets the Eye
In addition to the ultrasound curriculum, USASK medical students benefit from the efforts and hard work of the USASK Ultrasound Interest Group as well as the annual SASKSONO conferences (established in 2016).

The U of S Ultrasound (USUS) student group provides additional scan time to students throughout the year. This student-led group provides a low-pressure environment for medical students to reinforce scanning techniques taught through the curriculum. The group hosts “scan-night” sessions on-campus. Students have the opportunity to practice on each other and gain additional time with the probe in hand. Approximately 40 students attend each scan night and students are given one hour to practice each night. The group hosts around five events per year. A notable event for the group is the OSCE review night which focuses on preparing students for an OSCE station requiring the use of ultrasound. In previous years the OSCE review night has had more than 60 attendees. A great review of USUS can be found here.

Our annual SONO-conference explores the role clinical ultrasonography in improving patient outcomes and system efficiencies. Our conferences include a range of learning experiences including short lectures, hands on workshops for beginners as well as those already familiar with the basics, supervised scanning with top level coaching, as well as rapid oral abstracts and the always entertaining SONOlympiad. Check out the details from our previous 4 conferences here.

Overall, we would grade the USask ultrasound curriculum as a B+. The sessions themselves include the majority of the CanUCME recommended curricular elements and are delivered efficiently.
Room for Improvement
The College of Medicine at the University of Saskatchewan already meets most objectives and is working to integrate outstanding items in order to improve the delivery of the Clinical Ultrasound teaching. Currently, gaps in respiratory ultrasound (specifically B lines, consolidation, and pneumothorax) are being addressed through new modules at the clerkship level (core EM rotation).
Student Feedback
Moreover, we analyzed student feedback and found that a point for improvement relates to the frequency of ultrasound sessions. Students consistently self-rated their ultrasound skills as poor before a teaching session, but described significant improvement afterwards; nevertheless, their improvement was felt to be largely lost by the time the next teaching session occurred the following term. We feel the curriculum could slow this perceived regression by implementing more frequent scanning sessions. This infrequency was the most commonly commented critique during session evaluations: students want more ultrasound sessions.
While students strongly appreciated and valued the audiovisual learning materials that accompanied ultrasound teaching sessions, students frequently noted in evaluations that they would appreciate more concise reference material. We suggest digital visual aids/summaries that outline the correct probe position, along with the appropriate landmarks for each scan. In turn, students will have a concise means of reviewing before quizzes and OSCEs. The final area we recommend for improvement is increasing POCUS exposure in other core rotations such as pediatrics, anesthesia, general surgery and family medicine.
Conclusion
The USask US program has gradually taken shape over the course of several years, guided by local expertise, support from university administration, and most recently, the CanUCMe’s recommendations. The program has established a number of longitudinal training strategies delivered in class and on rotation with both real and standardized patients. The curriculum meets nearly all of the of the curricular elements of the CanUCME recommendations. Ultrasound relating to the respiratory system and opportunities for hands-on self-directed learning are areas for improvement. As the use of ultrasound continues to grow and clinical ultrasonography becomes more prevalent in clinical practice, we encourage our peers at other institutions to evaluate their own ultrasound curriculum as a means of bringing all Canadian medical schools in alignment with expert-guided standards such as the CanUCME recommendations.
Authors
Mars Zhao, Michael Durr, and Michael Thatcher are in their 2nd year at the College of Medicine at USASK
Dr. Paul Olszynski is the lead for UGME Ultrasound at the University of Saskatchewan, and Dr. Ali Turnquist is a regular POCUS instructor and lecturer with the UGME Ultrasound program.
External Reviewers
Dr. Irene Ma (University of Calgary) and Dr. Brian Buchanan (University of Alberta)
References

The COVID19 pandemic has had profound effects on healthcare delivery and education. From the clinical side, we see yet again how POCUS plays an important role in patient triage, assessment and monitoring. From the education side, we are seeing a swell of interest in simulation not only as a teaching technique, but also as a process testing tool that can help refine our approach to novel challenges in acute care. As we move into the next phases of the pandemic, both POCUS and simulation will continue to play their roles.
From a teaching perspective, as we adapt some of our students’ clinical experiences during the pandemic, increased use of simulated clinical care seems reasonable. With that in mind, we are thrilled to release our newest update of USASK’s Emergency Department UltraSound Simulator (edus2), now downloadable to any windows laptop and much easier to use through the power of Java!
If you want to run edus2j on your laptop (for your sim lab, or small group teaching sessions, in-situ sim, wherever) here are the steps:

Assemble a transducer and purchase RFID tags using our instructions on the GitHub page or contact sasksonic@gmail.com to order a transducer (built from a hollowed deodorant stick as seen above). You can run the program on any windows-based laptop (it will take up about ~ 100MB all total)

Once the hardware is ready, plug in the probe and create an edus2 folder on your desktop. In that folder, create sub-folders for 1) video library 2) saved scenarios 3) saved mannequins

Download Java: https://www.java.com/en/download/
Download edus2j: https://github.com/camauser/edus2j/releases/download/1.3/edus2j.jar
Download our edus2 video library: https://www.dropbox.com/sh/55zd96yda694amc/AACcsAV2kYtXhMlS8QO1ec_ka?dl=0
Then watch our instructional videos:
1Watch video 1 on downloading Java and the edus2j program onto your computer (for free) https://vimeo.com/427519450
2. Watch video 2 on running the simulator, designating mannequins, and uploading videos https://vimeo.com/427519524
3. Video 3 creating scenarios and exporting mannequins. https://vimeo.com/427519597
Let us know if you need a hand!
cheers,
Cameron Auser, BSc @camauser
Malcolm Whyte, BSc
Paul Olszynski, MD @olszynskip
Huge thanks to the team at the USASK CLRC for their patience and feedback during beta testing!
CAEP will be releasing a formal document shortly but in the meantime, here are some key considerations:
A) Is the scan clinically indicated and will the results change management?
POCUS Preparation and cleaning in AGMP rooms.
B) Do i have time to properly drape the machine and then clean it afterwards?
Take cleaning and preparation time into consideration as you decide whether or not you will use POCUS. As the list shows, you are looking at an additional 10 minutes for preparation and cleaning. Also – now is generally not the time to learn totally NEW POCUS applications. The use of a COV-19 lung protocol (linked below) is within the scope of any credentialed POCUS user and may be helpful when conventional imaging like CXR are limited.
C) Should i get a handheld POCUS device since they are easier to clean?
Health Canada has recently approved the newest handheld devices (Butterfly IQ) in light of the pandemic (and how much more easily they can be cleaned). Some departments are buying these in large numbers. My understanding is that these departments (some in Sask) have clearly defined the use and cleaning parameters for these devices. With the right processes and procedures in place , we can keep our staff and patients safe during these very challenging times.
Should you have any question, please don’t hesitate to connect sasksonic@gmail.com


There has been A LOT of talk about POCUS governance lately – and at USASK we are right in there with a recent publication in The Ultrasound Journal on our efforts to develop a consensus-based multidisciplinary POCUS framework.
This Saturday @USASKEM and @usask_CME are hosting the 11th Saskatchewan Emergency Medicine Annual Conference (SEMAC XI) in Saskatoon, SK. We will be reviewing the recently adopted (province wide) Saskatchewan Emergency Ultrasound Guidelines: STANDARDS FOR EMERGENCY ULTRASOUND Final
These are in keeping (and in fact exceed) the above USASK POCUS Framework and are also well aligned with CAEP’s recent EM POCUS Position Statement.
Here’s the Executive Summary for the Sask EUS Guidelines:
Emergency ultrasound (EUS) comprises a set of focused applications utilized to diagnose life-threatening conditions, guide invasive procedures, and treat emergency medical conditions. [2] The proposed standards take into account that emergency care, and thus EUS, is within the scope of emergency physicians, family physicians and nurse practitioners. Given the significant contextual and resource differences between urban/tertiary centres and rural/regional sites, recommendations related to training, privileging and quality assurance are tailored accordingly.
These standards represent one of many initiatives developed to help ensure high quality training in, and use of, EUS in the province of Saskatchewan.

The USASK experience with logging scans and the EchoLog App
|

Big thanks to out-going USUS President Laura Neuburger for submitting this review!
Click on the link for a copy of the update: USUS 2018-2019 Update
We’re excited to be announcing the following fall courses:
The EDE course in Saskatoon, SK on Sept 22nd, 2019.
The EGLS Course in Saskatoon, SK has been scheduled for Oct 7th/2019.
To register or get more info, contact sasksonic@gmail.com

Stay tuned – details including dates and presenters will be coming soon!
REGISTRATION NOW OPEN: https://ccdeconference.usask.ca/index.aspx?cid=408
This year, our “DEEP DIVE” means we will be going beyond test performance metrics, exploring in-depth the role clinical ultrasonography can have in improving patient outcomes and system efficiencies. Our conference includes a range of learning experiences including short lectures, hands on workshops for beginners as well as those already familiar with the basics, a Sono-Round Table to develop a multidisciplinary clinical ultrasonography framework at USASK, supervised scanning with top level coaching, as well as rapid oral abstracts and the always entertaining Sonogames!
As organizers, we are committed to delivering a conference that supports the learning and wellness of all our attendees. We have included several optional opportunities for networking, exercise, relaxation and laughter! We will also have spaces for breastfeeding/pumping for those who may choose to use them, and as organizers, will do our best to help attendees secure quality childcare if needed. We also hope to be a low/minimal waste conference so please consider bringing your own coffee mug and/or water bottle.
7:30: Wellness Opportunity (optional) “Run at the speed of sound” or “Sound walk with talk”. We will provide a meeting location and encourage our attendee runners and walkers to join us for a great start to the day!
8:00 – 9:00 am: Registration and breakfast
9:00 am: Introductions and acknowledgement of our Treaty 6 commitment.
9: 15 am: Dan Kim – Deep Dive into EM POCUS
9:45 am: Dr. Peggy Lambos – Deep Dive into Pediatric POCUS
10:15 am: Nutrition break (Wellness oriented with healthy snacks offered)
10:30 am – 12:00 pm: Morning Concurrent Sessions
FUNdamentals: POCUS 101 will be an introductory session for those new to clinical ultrasonography/Point of Care Ultrasound (POCUS). It will include flipped content sent to you before the conference as well as a quiz. The workshop will include a brief review ovf key concepts and hands on scanning practice of three core applications: scanning for abdominal and pleural fluid as well as pericardial effusion. Completion will include an assessment which, if passed, makes you eligible for more supervised scanning in the afternoon!
PROfound: USask’s first ever multidisciplinary POCUS Round Table will give Saskatchewan clinicians a chance to further guide the adoption and integration of POCUS throughout the province of Saskatchewan. We hope to establish provincial recommendations on training, scope of practice, documentation and quality assurance. Key recommendations will then be shared with the entire conference audience at the last session of the day for feedback and ratification. There will be flipped content sent out for this session including a draft framework document.
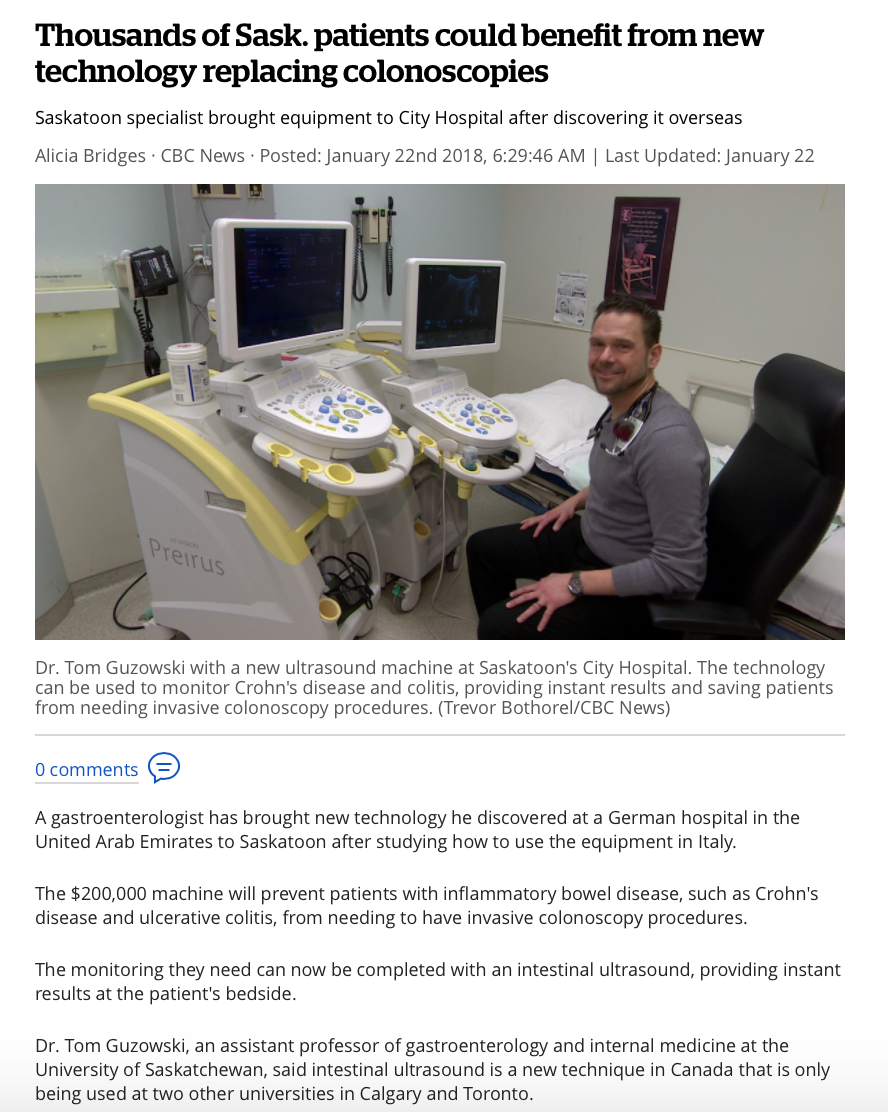
SONO EXPO: For those interested in exploring the spectrum of POCUS applications at USASK, we are excited to offer you deep dives into Inflammatory Bowel ultrasound as well as Pediatric EM ultrasound. And as usual, expect at least 30 minutes of hands on scanning and anatomy learning as well! This is a great opportunity for students and residents to explore applications outside the core USASK POCUS curriculum.
12:00 pm – 1:00 pm: Break which includes a nutritious lunch, an optional stretching session, opportunities to connect with old friends and/or make new ones!
1:00 – 4:00 pm: Afternoon Concurrent Sessions
SONO Abstracts and SONOlympiad: Always inspiring, educational and a good time, the students square off with their abstracts and then go head to head in the sonogames.
1:00 pm: SonoAbstracts

2:00 pm to 3:45 pm : SONOlympiad
SUPERVISED SCANNING: Struggling with an application or two? Need some POCUS coaching? Here’s your chance! Instructors qualified in basic, diagnostic and resuscitative POCUS will be on hand to help you take your scanning to the next level for 3 straight hours! And if that seems a bit daunting – don’t sweat it, we’ll offer a mid-point stretch and re-energizing session. This way you’ll be sure to finish strong as you head into the final hour which will include (for section 3 credits) a detailed assessment of your skills!
4 pm: Closing session
SONO ROUND UP: We will present the main recommendations for a USASK POCUS Framework as developed by the Round Table panels and participants. The audience will have the opportunity to provide feedback and vote using an audience response system.
REGISTRATION NOW OPEN: https://ccdeconference.usask.ca/index.aspx?cid=408

CHECK OUT THE TRAILER!
Download the poster (with an active registration link) for distribution to your colleagues!
As the role of clinical ultrasonography continues to grow throughout healthcare, the need for clear communication of bedside findings has never been greater. We know that communication plays a major role in high quality healthcare, and that miscommunication has been identified as a major contributor to medical error and patient complaints.
Last year at SASKSONO17 (Breaking the Sound Barrier), we discussed the need for clear communication amongst clinicians. Our panel of experts (Internist, Intensivist, Emergentologist and Hospitalist) offered great advice on how best to communicate clinical ultrasound (aka POCUS) findings with colleagues and consultants (you can check out the 8 minute video here: https://vimeo.com/215476593).
But clear communication with colleagues is only one piece of the puzzle. The other big piece is clear communication with the patient! And while this may seem self-evident, we suggest there’s more to it than simply applying basic clinician-patient communication skills. For example, I am sure you have heard a trainee or colleague say to their patient, after having completed a bedside scan, that everything looks OK. Seems harmless doesn’t it? But to the patient, there is now a very real potential for misinterpretation of both the purpose of the scan, and the findings! Here at Sasksonic we’ve heard it first hand. Patients have returned to their primary care providers with impressive stories of whole body scans where their liver, spleen and kidneys were evaluated by ultrasound and “Great news doc, everything was OK!”
By not clearly stating the indications for the scan, or not clearly explaining the findings, clinicians may give their patients the wrong impression that they have undergone a much more comprehensive evaluation than intended or necessary. This can lead to a lot of headache and frustration by downstream providers who now find themselves rummaging through the patient’s medical record looking for the “whole body scans” (assumed to be either consultative ultrasound or CT scans) when no such studies were performed. Furthermore, in the absence of a consultative report (or worse yet, no comments regarding to the point of care ultrasound in the visit note), it can also negatively impact the status of clinical ultrasonography in the eyes of our colleagues and patients. As an important and evidence-based part of the clinical assessment (now proposed to be the 5th pillar of the bedside assessment – inspection, palpation, percussion, auscultation and insonation), we need to ensure our colleagues and patients understand the role clinical ultrasonography plays in patient care.
The solution?
Whenever possible, clearly communicate with patients about the indications, findings and limitations of the clinical ultrasound scan in question. When performing a FAST scan this means letting the patient know you are looking for free fluid in the abdomen or chest, which if seen, would suggest internal bleeding. If no free fluid is seen, instead of saying “everything looks OK” we suggest you say “I don’t see any free fluid on my scan, but this clinical application of ultrasound has limitations and sometimes we miss injuries. Keeping the clinical picture in mind, I think we should proceed with…”
And there’s more! Whenever possible, be sure to give the patient a clear understanding of what the scan will include including where the transducer will be placed. Be sure to warn them about the room temperature gel that often feels ice cold. Then, while scanning, try to talk them through the findings as much as possible (this gets easier as your image generation skills improve). For example, when scanning the gallbladder for suspected cholelithiasis, take time to show them their gallbladder, what the wall looks like and whether there are any stones. Remember, one of the advantages of clinical ultrasonography is that you are learning about your patient’s (patho)physiology in real time at their bedside. So let the patient know what’s going on in the moment, tell them in a way they will understand, and quell their curiosity while also empowering them!
For an example of good communication with a patient (and other aspects of ultrasound etiquette) , check out this short clip we’ve prepared at Sasksonic for our trainees.
https://player.vimeo.com/video/270078460
cheers,
Paul Olszynski and Qasim Hussain
Peer Review: Drs. Kish Lyster and Irene Ma

Congrats to “No Pain, No Gain”, our first place team at this year’s SASKSONO conference! Big thanks to all of our participants and to the crowd for cheering the teams on as they battled it out. Also big thanks to Dr. Quinten Paterson (PGY2 EM) and Ms. Alixe Dick (MS2 USASK) for their hard work in preparing the games this year and Drs. Kawchuk and Jelic for their sound judgment!
All in all, a very successful SASKSONO18 – We hope to see you next year at SASKSONO19!

Great news! We’re hosting an IP Core SKanapalouza for Rural and Regional Clinicians on March 10th!
This ultrasound scanning day is to facilitate clinicians seeking to obtain their Canadian Point of Care Ultrasound Society (CPoCUS) CORE Independent Practitioner certification. The intent is to provide clinicians working in rural areas an opportunity to obtain scans towards their certification that are otherwise difficult to achieve in such locations. There will be an opportunity to obtain up to 28 scans towards your certification. All standardized patients will be female to allow for maximum scanning applications. There will be a high instructor to participant ratio to ensuring a quality scanning opportunity.
For more details and to register, click on this link
cheers,
The Sasksonic Team

Continue reading the full article here

As we wrap up another great year at Sasksonic, we are thrilled to learn that one of our own recently took home POCUS-Toronto’s “Case of the Year” award!
USask EM’s Dr. Puneet Kapur (PGY5 EM, @Kapurp) was recognized for his stellar case submission involving identification and test performance of several transthoracic echo findings as they relate to identifying acute pulmonary embolism. Many of you have heard of the value of each of the following findings as they relate to distinguishing acute from chronic RV strain: 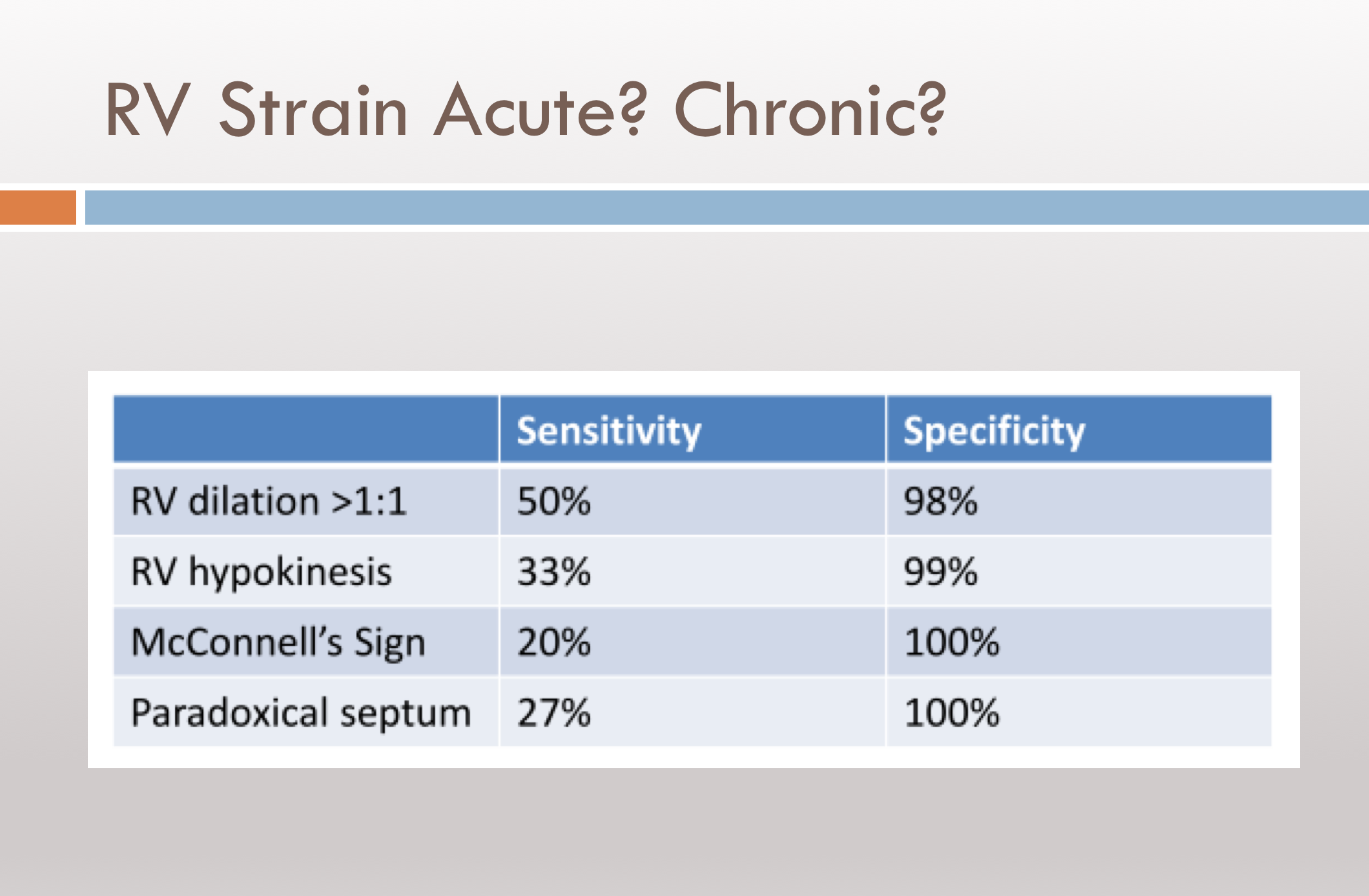
Here are clips from the actual case that show RV dilation in the PSL and McConell’s sign in the A4C. Despite these – it may remain challenging to reliably determine acute vs chronic strain (see details in the cited article below).
Well, don’t give up hope – introducing RVOT systolic excursion! This measurement is obtained using the parasternal short axis view at the level of the aortic valve.
 It appears that measuring RVOT systolic excursion (as a percentage of end-diastolic RVOT diameter minus end-systolic RVOT diameter divided by end-diastolic RVOT diameter) is both specific and highly sensitive for acute PE. Analysis of right ventricular outflow tract systolic excursion showed that a value <24.3% can be found in acute pulmonary embolism patients with 100% sensitivity and 95.56% specificity (AUC = 0.987, P < 0.0001).
It appears that measuring RVOT systolic excursion (as a percentage of end-diastolic RVOT diameter minus end-systolic RVOT diameter divided by end-diastolic RVOT diameter) is both specific and highly sensitive for acute PE. Analysis of right ventricular outflow tract systolic excursion showed that a value <24.3% can be found in acute pulmonary embolism patients with 100% sensitivity and 95.56% specificity (AUC = 0.987, P < 0.0001).
Sounds promising – looking forward to hearing and learning more about this.
We’re proud of Puneet! And while we’re at it – big thanks to the team at POCUS-Toronto for giving trainees like Dr. Kapur an opportunity to learn and excel in emergency POCUS.
Want to learn more about RVOT systolic excursion and acute RV strain? Check out the article below:
Placing a line with ultrasound? Blocking a nerve? Checking for pneumothorax? Assessing LV function? Confirming intra-uterine pregnancy? Sorting out shock with TEE?
EVERYTHING IS POCUS!
Meet our amazing faculty from Internal Medicine, Critical Care, Emergency Medicine, Pediatrics, and Paramedicine! Join us for engaging lectures, productive workshops, and hands-on coaching!

Detailed conference agenda found here: schedule_sono20
As always, we’ll be hosting our annual SONOlympiad where our medical students compete for the SonoCup!

To register your team – details are as follows:
Teams of 3-4 should submit a 5-10 minute creative video highlighting:
– member skills (clips of scanning or image interpretation)
– team name and outfits
– unique team strengths
Content covered at this year’s games is listed within the proposed Canadian Medical Student Ultrasound Curriculum by Ma et al. https://doi.org/10.1002/jum.15218 (specifically Table 4)
Team videos should be submitted to sasksonic@gmail.com
Selection Criteria:
– clear demonstration of image generation skills (clip shows team member scanning while also showing the POCUS image all in a single frame) with the above curriculum in mind
– case integration to show knowledge of indications and how to integrate findings with the above curriculum in mind
– creativity
– team name
– unique team strengths?
Submission deadline will be March 9th.